Subscribe if you want to be notified of new blog posts. You will receive an email confirming your subscription.
Details “Emerge” on the Medicare Medical Home Demonstration
Where would one expect to find CMS’ latest thinking on the upcoming Medicare Medical Home Demonstration project? The obvious answer would be “on the Official CMS MMHD home page ”, but you’d be wrong.
CMS has issued a Medicare Medical Home Demonstration Payment Contractor RFP available on the Federal Business Opportunities website. Thanks to the Google Alert service for digging this out.
For the casual reader, the details of the MMHD are taking shape nicely. CMS and its advisors have obviously spent a lot of time planning for this tremendously important project. If successful, the MMHD can salvage primary care from the jaws of death, rationalize reimbursement policy, and set the world right. Other than that it’s business as usual.
For those of you interested in how the details are unfolding, read on…
The MMHD Payment Contractor RFP has links to 20+ documents, most of which are mumbo jumbo contracting details. Here’s where I found the most useful information describing MMHD developments:
- Statement of Work (SOW), authored by CMS
- Design of the CMS Medical Home Demonstration , authored by Mathematica Policy Research, the Center for Health System Change (CHSC), and the National Committee for Quality Assurance (NCQA); June 19, 2008
These documents carry differing weight. I interpret the SOW as CMS itself speaking — that representations in this document reflect decisions CMS has already made. In contrast, the Mathematica/CHSC/NCQA Design Report represents input from CMS advisors, which CMS could choose to follow or not. We’ll know for sure when the final RFP for the MMHD comes out.
Let’s look at the Statement of Work and the Mathematica/CHSC/NCQA documents separately.
From the Statement of Work Document
There are a few points worth noting:
Scope of the MMHD.
The number of physician practices that will participate in the demonstration is estimated at 400; we estimate this will result in approximately 2,000 individual physicians participating. Each practice is estimated to serve 200 beneficiaries resulting in about 400,000 beneficiaries that could participate over the course of the demonstration. The Payment Contractor shall make payments to qualified Medical Home practices in eight demonstration locales (to be determined at a later date).
This is big. It suggests that CMS is taking this demo very seriously.
Physician Practice Qualifications. It’s looking like CMS will have fairly rigorous qualifications for physician participation.
The qualification process will be similar to that used by the National Committee for Quality Assurance in the Physician Practice Connections-Patient-Centered Medial Home program.
This is a two edged sword — it’s good that the definition of “medical home” has some rigor and specificity; yet, too much rigor could dissuade physicians from undertaking steps to qualify and participate in the demo.
Risk Adjusted Payments. As I’ve written previously , the care management fee is one of the most important and poorly defined aspects of the Medical Home model. The reimbursement methodology recommended by the American Medical Association/Specialty Society RVS Update Committee (RUC) last spring was met with confusion and outrage. To refresh your memory, read here , here , here , here , here , here , here , here , here and here .
I’ve also shared my perspectives that using the RUC methodology is entirely inconsistent with the principles underlying the Medical Home model. The RUC methodology only measures inputs (primarily physician and nurse labor), while a valid Medical Home reimbursement approach should be based on value created (outputs).
The RUC methodology made no provisions for risk adjustment of fees based on severity of patient illness. In the SOW document, CMS explicitly states it will use risk adjustment in the MMHD:
Individual payments will be risk adjusted based on a methodology established by CMS
Risk adjustment goes a long way toward undoing the potential damage of using the RUC methodology. Risk adjustment provides incentives for physicians to provide adequate care coordination for all patients, and not to avoid dealing with the sickest patients that require a disproportionate amount of time.
Many physicians — particularly geriatricians — actually LIKE to care for frail elderly patients. We need more — MANY MORE — of these doctors. Risk adjustment will avoid penalizing physicians that want to attract frail elderly patients to their practices.
Mathematica/CHSC/NCQA MMHD Design Report
There’s some really good thinking in here.
The document is well organized and addresses:
- Basic Features of the MMHD — What is a Medical Home? Which physician practices are eligible? Which Medicare beneficiaries are eligible? How are participating practices reimbursed?
- Demonstration Procedures — What is the demonstration timeline? How will demonstration sites be selected? How will physicians be recruited? How will physician practices apply and become enrolled? How will beneficiaries become enrolled? How will patient and physicians transitions during the demonstration be handled? How will practice qualifications be measured, verified, and monitored? How will the demonstration be evaluated?
Here are some of the design recommendations that I found particularly noteworthy.
Beneficiary Eligibility . The enabling legislation specified that the MMHD focus on “high need populations”, defined as “individuals with multiple chronic illnesses that require regular medical monitoring, advising, or treatment”.
Previous Medicare disease/care management demos have focused on the top 2–5% high cost/risk beneficiaries, and I had assumed that the MMHD would be directed at a similar population.
However, the Mathematica/CHCS/NCQA report is defining “high need” quite broadly for the purposes of the MMHD. Using the recommended definitions, about 86% of Medicare beneficiaries will be eligible (p.10).
While this is a stretch from the original legislation, it makes a lot of sense to open up the MMHD to almost all Medicare beneficiaries:
- Recruiting physicians will be easier. Physicians would have little incentive to participate if only a handful of their sickest patients were taking part in the MMHD.
- Recruiting patients will be easier. Within the participating physician practices, enrolling in the MMHD will become mainstream.
- The MMHD takes on a much more preventive/wellness orientation. Counter to expectations, one of the lessons learned in Medicare Health Support was that the greatest cost savings opportunities were NOT with the very sickest population — that these patients were already on unchangeable trajectories due to illnesses and health habits ingrained over the course of a lifetime.
Physician Practice Reimbursement . CMS will share the savings with participating practices only if the estimated savings exceeds 2% of the comparison group costs.
Practice reimbursement will not depend on quality of care indicators. Note that this is 100% at the other end of the spectrum from the Physician Group Practice demo, which ties physician incentive payments exclusively to quality improvements.
Demonstration Timeline:
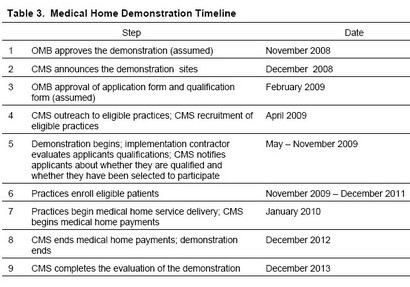
Click here to see a larger version of the timeline.
Selection of Demonstration Sites . There are a couple of notable points here.
First, unlike many other demos, the sites will be geographically bound and limited to eight sites (no smaller than a county, no larger than a state). This could make physician practice recruitment difficult; practices that might be highly interested in participation won’t be eligible unless they are located in one of the chosen sites.
Second, the Mathematica/CHCS/NCQA report opens the door to a possible multipayer initiative in locations where private insurers are also testing medical home initiatives. This is an interesting twist.
Beneficiary Enrollment. Physicians will be expected to enroll patients directly. In other Medicare disease/care management demos, enrollment has been challenging — enrollment typically has been performed by a 3rd party, e.g., a DM company or a health plan that has had no previous relationship with the Medicare beneficiary.
Enrollment processes in the MMHD should be fairly straightforward due to the preexisting doctor patient relationship — patients will likely take their doctor’s recommendation to enroll without much questioning.
These are a few initial reactions to two documents with a lot of meat in them…your comments and perspectives are welcomed.
This work is licensed under a Creative Commons Attribution-Share Alike 3.0 Unported License. Feel free to republish this post with attribution.
How do i find the 8 demonstration sites and geographic locations? Also, how do I enroll into the demonstration project?
Kimberly,
The project is behind schedule. I don’t believe the sites have been announced.
The MMHD homepage is:
http://www.cms.hhs.gov/DemoProjectsEvalRpts/MD/itemdetail.asp?filterType=none&filterByDID=-99&sortByDID=3&sortOrder=descending&itemID=CMS1199247&intNumPerPage=10