Subscribe if you want to be notified of new blog posts. You will receive an email confirming your subscription.
HIPAA

Health Data Outside HIPAA: Simply Extending HIPAA Would Be a #FAIL
Health Data Outside HIPAA: Simply Extending HIPAA Would Be a #FAIL

Protecting Health Data Outside of HIPAA: Will the Protecting Personal Health Data Act Tame the Wild West ?
Congress is seriously considering bipartisan legislation — the “Protecting Personal Health Data Act” — to better protect the privacy of consumers’ personal data.

Health Data Outside HIPAA: The Wild West of Unprotected Personal Data
The average patient will, in his or her lifetime, generate about 2,750 times more data related to social and environmental influences than to clinical factors.
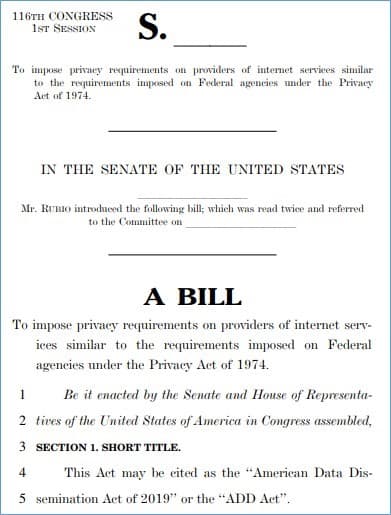
For Your Radar — Huge Implications for Healthcare in Pending Privacy Legislation
The U.S. Congress is considering broad privacy and data protection legislation in 2019. There is some bipartisan support and a strong possibility that legislation will be passed. Federal privacy legislation would have a huge impact on all healthcare stakeholders, including patients.

Hoarding Patient Data is a Lousy Business Strategy: 7 Reasons Why
In the video below, Dr. Harlan Krumholz of Yale University School of Medicine capsulizes the rationale of hoarding as business strategy:
We encourage you to take a minute to listen to Dr. Krumholz, but if you’re in a hurry we’ve abstracted the most relevant portions of his comments:
“The leader of a very major healthcare system said this to me confidentially on the phone… ‘why would we want to make it easy for people to get their health data…we want to keep […]

Editorial: A Duty to Share Patient Information
by Vince Kuraitis and Leslie Kelly Hall, Senior Vice President, Policy, Healthwise.
The sharing of patient information in the US is out of whack — we lean far too much toward hoarding information vs. sharing it. While care providers have an explicit duty to protect patient confidentiality and privacy, two things are missing:
the explicit recognition of a corollary duty to share patient information with other providers when doing so is the patient’s interests, and
a recognition that there is potential tension between […]

List of Top 10 Health Plan Issues — Out of Whack!
Healthcare IT News just published its list of top issues for health plans in 2011:
Administrative Mandates (Compliance HIPAA 5010, ICD-10, etc.).
Care Management, Data Analytics, and Informatics.
Health Insurance Exchanges and Individual Markets.
New Provider Payment & Delivery Systems (ACOs, PCMHs, etc.).
Bend the Cost Trend.
Medicare and Medicaid.
Health Information Exchanges and EMRs.
Consumer’s Role in the Modernization of Healthcare.
Reform Uncertainties.
Payer/Provider Interoperability.
Dear health plan colleagues,
Wake up! The order of this list is totally out of whack.
#2: Care Management, Data Analytics, Informatics. Good…sounds about right.
However,
#2 can’t […]

Crowdsourcing the Future: Health 2.0 and HIPAA
Deven McGraw is the Director of the Health Privacy Project at the Center for Democracy & Technology.
The Health 2.0 movement has seen incredible growth recently, with new tools and services continuously being released. Of course, Health 2.0 developers face a number of challenges when it comes to getting providers and patients to adopt new tools, including integrating into a health system that is still mostly paper-based. Another serious obstacle facing developers is how to interpret and, where appropriate, comply with […]

Walled Gardens vs. the Open Web: A Central Debate in Tech Finally Coming to Healthcare
The September issue of Wired magazine and an article in last Sunday’s New York Times illustrate a central debate in technology circles. The debate is not new — it’s being going on for two decades — but it has newfound vibrancy. The essence of the debate is about competing tech/business models: walled gardens vs. the open world wide web (web).
vs.
The debate is highly controversial and nuanced. There are “experts” on both sides.
My point today is not to take sides […]

Digital Medical Office of the Future Conference. Las Vegas, Sept. 9-10
CLICK HERE FOR THE CONFERENCE WEBSITE
Healthcare providers face critical choices in selecting and implementing Electronic Health Records (EHRs). In addition, physicians and hospitals will need to develop the capacity to exchange clinical information in order to meet Meaningful Use requirements. This program will offer detailed and practical information on EHR selection and implementation, as well as strategies for creating a sustainable health information exchange (HIE). The program also features sessions on legal/regulatory issues, clinical platforms and applications as […]