Subscribe if you want to be notified of new blog posts. You will receive an email confirming your subscription.
The Missing Ingredient in Today’s Patient Portals: Network Effects
by Vince Kuraitis and Jody Ranck
As described in the first three posts in this series, today’s patient portals are inherently flawed and doomed to mediocrity. The result is that today’s patient portals cannot achieve a critical mass of adoption and utilization, and therefore portals can’t achieve network effects.
In this post, we will:
- Summarize key points from the first three posts in this series
- Explain how today’s patient portals miss out on three types of network effects
- Explain the implications: why tomorrow’s portals must be reconfigured to achieve network effects
Summarizing
Let’s review some of the key points from the first three posts in this series.
Patients would prefer one portal “home” (from the 1st post in this series):
By definition, today’s portals are NOT patient-centric—they are tethered to individual provider organizations.
Today’s patient portals CAN NOT achieve their potential because patients do not want multiple portal “homes”. Your mom would prefer to have one portal, NOT seven.
Patient portal adoption and usage has been tepid. The ONC survey found that 59% of patients reported having been offered a portal in 2020 and that 38% had actually used one.
When patients were asked how they used their portal, most of the reported use was transactional–as opposed to being relational and/or used as part of a longitudinal clinical care process. As reported by 86% of respondents in 2020, the single greatest use of a portal was simply to review test results.
The single greatest benefit from the hospital POV was “accepting patient payments”, cited by 94% of respondents. Only 35% of hospital execs saw value in involving patients in their clinical care.
Today’s portals capture stand-alone value, NOT network value (from the 2nd post in this series):
Today’s patient portals can provide some stand-alone value, but they provide minimal network value.
Stand-alone value refers to the value provided by an offering that is independent of how the platform is used by others, e.g., your PC being used solely by you to create a word-processing document, a spreadsheet, or to play a single-player video game.
Your PC gains network value–value created through the activity and usage of others–when connected to the internet or another network. Now, you can share documents with colleagues and collaborate in editing. You can work together on spreadsheets. You can play multi-player games in real time.
Portals offer mostly stand-alone value — the ability to conduct discrete transactions within one provider organization, e.g, to pay bills, to check on a lab result, to request a prescription.
Today’s patient portals can not provide network value because they are tethered to single institutions or care providers.
Most patients see a wide range of providers. One study found that only 5% of Medicare patients have records with only 1 vendor and that 20% have medical records w/ 8+ vendors.
Patients can come for the tools…but there’s no network to stay for.
Multiple portals results in high friction for patients (from the 3rd post in this series):
Patients who use multiple portals inevitably encounter friction: multiple signups, differing UI’s for different portals, varying functionality across portals, non-standardized clinical terminology, non-standardized data, the lack of one care plan, and uncertainty regarding follow-up care.
This friction is more than inconvenient for patients—it’s dangerous to their health and safety. There’s no practical way for patients OR providers to reconcile and integrate information and workflow.
The Result: Today’s Portals Can’t Achieve Network Effects
Network effects are the phenomenon whereby a product or service gains additional value as more people use it. Due to the inherent flaws summarized above, today’s portals are unable to achieve a critical mass of adoption and growth, and therefore can’t trigger the network effects that are essential to platform success.
The importance of network effects in platform success can’t be overstated. NfX has calculated that network effects have been responsible for 70% of all the value created in technology since 1994.

The discussion around platform effects can become quite technical. For example, NfX has identified at least 16 types of network effects.
MIA: 3 Types of Network Effects
For now, we’ll keep it straightforward and take a look at three types of network effects that today’s patient portals aren’t able to tap: 1) Indirect network effects—patients and clinicians, 2) Indirect network effects—3rd party complementors (apps), and 3) Data network effects.
Today’s Portals Miss Out on “Indirect Network Effects—Patients and Clinicians”
This goes to the heart of patient portal failures—your mom would prefer one patient portal instead of seven. Your mom would value ALL of her clinicians being on the same portal.
Patients would value more clinicians being on the same portal. Their use of fewer portals would be more effective and efficient.
more clinicians >> more patients >> more platform usage >> more clinicians >>…
Clinicians would also value more patients using the portal. For example, workflow could be more consistent and integrated if a higher proportion of patients used portals; more manual tasks could be automated; patient clinical information could be provided and reinforced on a portal, and much more.
Today’s Portals Miss Out on “Indirect Network Effects—3rd Party Complementors (Apps)”
Today’s portals also are limited in their ability to tap network effects that could be created by 3rd party complementors. Developers who create apps for a platform can add functionality and value to the base platform.
As an example, Apple iOS and Google Android are the operating systems for smartphones They each have over 2 million apps that were created by 3rd party developers. The apps (complements) for these operating systems add tremendous value to the iOS and Android platforms.
Developers prefer to work with as few platforms as possible—typically one or two. That’s because there is a steep learning curve and significant and ongoing time and effort to learn how to develop for a platform. The competition for developers is a major factor that explains why the smartphone OS market consolidated from 12 platforms in 2006 to 2 winners (iOS and Android) by 2016.
In contrast, today’s patient portal software market is highly fragmented. Software Advice lists 59 different patient portal products. This paints an unattractive picture for 3rd party developers who potentially could add significant functionality and capabilities to patient portals. They will view almost all of these individual patient portals as having insufficient critical mass to justify the time and effort needed to create apps.
IQVIA’s Digital Health Trends 2021 documents that there are over 350,000 mHealth apps available to consumers. Can you imagine that many of these mHealth apps would function more efficiently and effectively if they were integrated into a comprehensive patient portal? We can.
Today’s Portals Miss out on “Data Network Effects”
Venture capitalist Matt Turck described data network effects:
Data network effects occur when your product, generally powered by machine learning, becomes smarter as it gets more data from your users. In other words: the more users use your product, the more data they contribute; the more data they contribute, the smarter your product becomes (which can mean anything from core performance improvements to predictions, recommendations, personalization, etc.); the smarter your product is, the better it serves your users and the more likely they are to come back often and contribute more data – and so on and so forth.
This diagram from CBInsights illustrates the positive feedback loop created by data network effects.
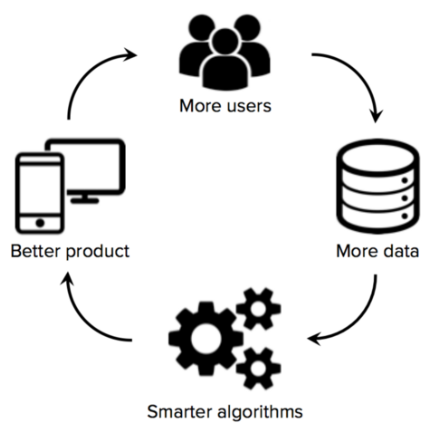
Today’s portals capture minimal & low-value data from patients. Current uses of portals are primarily administrative and transactional. How much data and how much value can be captured when a patient views a lab test or pays a bill? Not much.
The promise of portal data network effects lies in capturing data that is clinical and longitudinal across a continuum of care. Rich data can be used to improve patient care.
Implications: Tomorrow’s Patient Portals MUST Achieve Critical Mass and Network Effects
The implications are simple, but profound.
Today’s patient portals can not achieve a critical mass of adoption and usage, and therefore are unable to trigger network effects. Tomorrow’s portals MUST achieve critical mass and network effects
But how? That will be the subject of the next post in our series. While today’s portals CAN NOT work as configured, we’ll look at some alternatives that could work to reach critical mass and to create network effects.
“The single factor that separates a successful platform from a failed one is the development of network effects.” –Sangeet Paul Choudary
- Platform Terminology Explains Why Today’s Patient Portals CAN NOT Work
- Today’s Patient Portals CAN NOT Work: An Inability to Capture Network Value
- Today’s Patient Portals CAN NOT Work: Friction ACROSS Portals
- The Missing Ingredient in Today’s Patient Portals: Network Effects
This work is licensed under a Creative Commons Attribution-Share Alike 3.0 Unported License. Feel free to republish this post with attribution.